At The Brain and Spine Centre, we specialize in the diagnosis and surgical treatment of neurological and spinal disorders. Dr. Muhammad Aqeel Natt, a leading neurosurgeon in Lahore, provides advanced, safe, and compassionate care for patients.

Cervical Laminectomy
Cervical laminectomy is a decompression surgery used to relieve pressure on the spinal cord and nerves in the neck caused by spinal stenosis, disc–osteophyte complexes, or ligament overgrowth. At The Brain and Spine Centre, Dr. Muhammad Aqeel Natt offers cervical laminectomy at Farooq Hospital, West Wood Branch, Lahore, using modern techniques with or without fusion to achieve stable, effective spinal cord decompression.
Our goal is simple: decompress the spinal cord safely, prevent neurological decline, and improve neck and limb function.
What Is a Cervical Laminectomy?
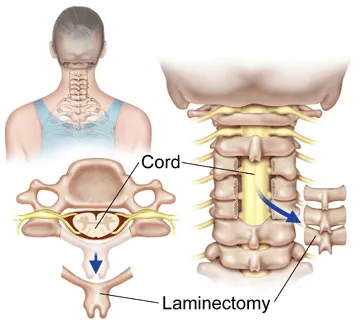
Cervical laminectomy is a posterior (from the back of the neck) operation in which the surgeon removes the lamina (the bony “roof” over the spinal canal) to create more space for the spinal cord and nerve roots. It is most often used for multilevel cervical spondylotic myelopathy or congenital stenosis when the cervical spine maintains normal or near-normal lordosis (natural forward curve). Laminectomy may be performed alone or combined with posterior fusion (laminectomy and fusion) to reduce the risk of post-laminectomy kyphosis and instability, especially in multi-level disease.
Symptoms and Indications
Cervical laminectomy is generally indicated for cervical myelopathy or severe stenosis affecting several levels.
Typical symptoms include:
- Hand clumsiness, difficulty with buttons, handwriting, or fine tasks
- Gait imbalance, leg stiffness, frequent tripping, or spasticity
- Non-dermatomal numbness or tingling in arms and/or legs
- Weakness in upper or lower limbs, often slowly progressive
- In advanced cases, bladder urgency or sphincter disturbance
Surgical indications include:
- Progressive signs and symptoms of cervical myelopathy despite conservative care
- Multilevel (≥3 levels) cervical stenotic myelopathy with preserved cervical lordosis or neutral alignment
- Compression from multilevel spondylosis, OPLL (ossification of the posterior longitudinal ligament), or ligamentum flavum hypertrophy not amenable to a limited anterior procedure
Diagnosis
Accurate diagnosis and surgical planning rely on clinical evaluation and advanced imaging.
- Neurological exam documents myelopathy signs, segmental deficits, gait changes, and long-tract signs.
- MRI of the cervical spine is the method of choice to identify canal stenosis, cord compression, T2 signal changes (myelomalacia), and alignment; it is essential for planning decompression.
- CT complements MRI by showing osteophytes, OPLL, and bony anatomy, helping to assess posterior decompression feasibility.
- Dynamic X‑rays (flexion–extension) assess instability and help decide on the need for fusion.
The Procedure
Cervical laminectomy is performed under general anesthesia with the patient prone.
Key steps:
- The neck is positioned to maintain or slightly increase lordosis, and the head is secured in a fixation system.
- A midline incision is made over the involved cervical levels, and paraspinal muscles are carefully elevated from the laminae.
- The laminae of the affected vertebrae (often 3 or more levels) are removed using high-speed burrs and rongeurs, decompressing the spinal cord and enlarging the canal.
- If laminectomy is combined with fusion, lateral mass or pedicle screws and rods are placed to stabilize the spine and maintain alignment.
- The wound is closed in layers, and a drain may be used temporarily.
Multilevel laminectomy is an effective and safe method of decompression in appropriately selected patients, but recognizing and addressing potential instability with fusion is essential.
Recovery & Aftercare
Recovery varies with age, pre-operative myelopathy severity, and whether fusion is performed.
- Hospital stay typically ranges from 2–5 days depending on comorbidities and the extent of surgery.
- Neck soreness and stiffness are common initially and gradually improve with physiotherapy; collars may be used short-term as directed.
- Walking usually resumes early, with gait and balance improving over weeks to months as cord function recovers.
- Formal rehabilitation helps restore neck mobility (within safe limits), upper limb dexterity, and gait, and reduces long-term stiffness.
- Long-term follow-up with clinical assessment and, when indicated, MRI is important to monitor decompression, fusion status, and adjacent segment health.
- Short‑term outcomes often show significant myelopathy improvement, but long‑term results can be influenced by age, pre-operative severity, and trauma. Older patients (>70 years), those with severe preoperative myelopathy, long symptom duration (>6–18 months), or trauma history have higher risk of delayed deterioration.
Results You Can Expect
When performed in properly selected patients:
- Cervical laminectomy (with or without fusion) can provide durable relief of myelopathic symptoms and halt disease progression in many patients.
- Long‑term studies show maintained improvement at 5 years, with some decline between 5–10 years related to age, trauma, or additional degenerative changes; average long‑term recovery rates around 30–60% have been reported depending on series and scoring system.
- Post-laminectomy kyphosis is common radiographically, particularly without fusion, but does not always correlate with neurological deterioration. Fusion reduces kyphosis risk at the cost of some motion and potential adjacent segment degeneration.
- Complication rates for posterior cervical decompression and fusion are reported around 15–25%. Common issues include blood loss anemia, wound infection, C5 palsy, and incidental durotomy acutely, and adjacent segment degeneration, junctional kyphosis, and pseudoarthrosis long term.
Why Choose The Brain and Spine Centre
Led by Dr. Muhammad Aqeel Natt, specialist spine and neurosurgeon experienced in cervical myelopathy management and multilevel posterior decompression with or without fusion. Use of high-resolution MRI and CT with modern grading of cervical stenosis to guide individualized surgical planning. Application of evidence-based indications—multilevel stenosis, preserved lordosis, progressive myelopathy—to maximize neurological benefit and minimize complications. Multidisciplinary postoperative care with physiotherapy, pain management, and long-term follow-up imaging to optimize functional recovery and spine health.
Cost of Cervical Laminectomy
Costs vary with the number of levels decompressed, whether fusion and instrumentation are required, hospital stay length, implants used, and rehabilitation needs. A personalized estimate is provided after consultation and review of imaging.
Frequently Asked Questions (FAQs)
Can I know Dr. Muhammad Aqeel Natt’s credentials?
What types of brain tumours do you treat?
Is the surgery safe?
Do I need long-term follow-up after surgery?
Are you having health problems? Contact us today!
Address Business
Contact With Us
Call Us 24/7: 0318 4065914
Working Time
Sunday: 8.30am - 19.30pm

