At The Brain and Spine Centre, we specialize in the diagnosis and surgical treatment of neurological and spinal disorders. Dr. Muhammad Aqeel Natt, a leading neurosurgeon in Lahore, provides advanced, safe, and compassionate care for patients.

Hydrocephalus
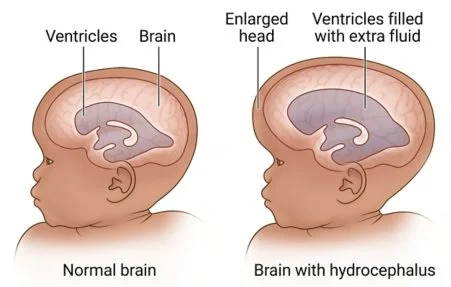
Hydrocephalus is a neurological condition in which cerebrospinal fluid (CSF) builds up abnormally inside the brain’s ventricles, increasing pressure on brain tissue and potentially causing serious, permanent damage if left untreated. At The Brain and Spine Centre, Dr. Muhammad Aqeel Natt provides advanced hydrocephalus care at Farooq Hospital, West Wood Branch, Lahore, including shunt surgery and endoscopic third ventriculostomy (ETV) for infants, children, and adults.
Our goal is simple: normalize CSF flow and pressure, protect brain function, and support the best possible quality of life.
What Is Hydrocephalus?
Hydrocephalus is an abnormal accumulation of CSF within the ventricles or CSF spaces of the brain, resulting from impaired flow, absorption, or rarely overproduction of CSF. CSF is continuously produced, circulates through the ventricles and subarachnoid spaces, and is reabsorbed into the bloodstream; disruption at any point in this system can lead to ventricular enlargement and raised intracranial pressure.
Major types include:
Congenital hydrocephalus: present at birth, often associated with neural tube defects (spina bifida), aqueductal stenosis, intrauterine infection, or genetic causes.
Acquired hydrocephalus: develops after birth due to hemorrhage, trauma, infection, tumors, or cysts obstructing CSF pathways.
Obstructive (non‑communicating) hydrocephalus: CSF flow is blocked within the ventricular system (e.g. aqueduct stenosis, posterior fossa tumor).
Communicating hydrocephalus: impaired CSF absorption at arachnoid granulations despite open pathways (e.g. post‑meningitis, subarachnoid hemorrhage).
Normal pressure hydrocephalus (NPH): usually in older adults, with enlarged ventricles and near‑normal CSF pressure; classically causes gait disturbance, urinary incontinence, and cognitive decline.
Symptoms of Hydrocephalus
Symptoms vary by age.
Infants:
Rapidly increasing head circumference, unusually large head, bulging tense fontanel (soft spot).
Prominent scalp veins, “sunset” eyes (downward gaze), irritability, poor feeding, vomiting, excessive sleepiness or lethargy, seizures.
Toddlers and children:
Headache (often morning‑worse), nausea and vomiting, irritability, lethargy.
Developmental delay, behavioral changes, decline in school performance.
Visual problems, papilledema, difficulty looking upward.
Gait disturbance, balance problems, urinary incontinence.
Adults:
Acute or chronic headaches, nausea, vomiting, blurred vision, balance problems, lethargy, cognitive decline.
In NPH: gait disturbance (magnetic, shuffling gait), urinary urgency/incontinence, and memory or thinking problems.
Any signs of raised intracranial pressure or NPH triad warrant urgent evaluation.
Diagnosis
Diagnosis confirms ventricular enlargement, identifies the cause, and assesses pressure.
MRI is typically the initial test in children and adults; it shows enlarged ventricles, periventricular edema, CSF pathway obstruction, tumors, hemorrhage, and congenital malformations. Fast MRI sequences can be used in infants without sedation.
CT scan is fast, widely available, and excellent in emergencies to detect ventricular enlargement, mass lesions, hemorrhage, or acute hydrocephalus, though it uses ionizing radiation.
Ultrasound through the fontanel is useful in infants to assess ventricular size and guide follow‑up.
Lumbar puncture / CSF tap test in suspected NPH assesses opening pressure and may be used prognostically; transient improvement in gait or cognition after CSF removal supports shunt responsiveness.
Treatment Options
Untreated hydrocephalus can be fatal; definitive treatment is surgical.
Ventriculoperitoneal (VP) shunt:
A VP shunt diverts CSF from a brain ventricle to the peritoneal cavity via a catheter and valve, where CSF is absorbed.
It is the most common treatment for hydrocephalus of all types worldwide.
Complications include shunt obstruction, infection, over‑drainage, under‑drainage, and need for revisions.
Endoscopic third ventriculostomy (ETV):
ETV is a minimally invasive procedure for obstructive hydrocephalus; using neuroendoscopy, a small perforation is created in the floor of the third ventricle, allowing CSF to bypass obstruction and flow directly into the basal cisterns.
ETV avoids implanted hardware; long‑term success is highest in aqueductal stenosis and some tumor‑related obstructions, and lower in infants with post‑infectious or communicating hydrocephalus.
Meta‑analyses show ETV has similar or better effectiveness and lower complication rates than VP shunting in selected patients with obstructive hydrocephalus.
ETV with choroid plexus cauterization (ETV‑CPC):
For selected infants, combining ETV with CPC reduces CSF production and improves ETV success, lowering long‑term shunt dependence.
Choice between VP shunt and ETV depends on age, etiology (obstructive vs communicating), ventricular anatomy, and prior infections or hemorrhage.
The Procedure
Our hydrocephalus pathway focuses on safe, durable CSF diversion.
Assessment: detailed history, neurological exam, imaging review, and, in NPH, gait and cognitive testing.
Surgical planning: decision for VP shunt vs ETV based on obstruction site, etiology, prior infection, anatomy, and local expertise.
VP shunt: small cranial incision and ventricular catheter placement, tunneled subcutaneously to the peritoneum, with a valve regulating CSF drainage.
ETV: endoscopic burr hole, navigation into third ventricle, and fenestration of its floor to create a new CSF outlet.
Postoperative care: monitoring for signs of over/under‑drainage, shunt malfunction, infection, and neurological improvement.
Recovery & Aftercare
Recovery is typically rapid after surgery, but lifelong vigilance is essential.
Many patients show rapid improvement in headaches, vomiting, and gait within days; NPH patients may improve over weeks to months.
Hospital stay ranges from a few days to a week, depending on age, comorbidities, and complications.
Regular follow‑up includes neurological assessment, head growth monitoring in infants, and imaging when clinically indicated.
Families are educated to recognize shunt malfunction/infection signs: headache, vomiting, lethargy, fever, wound redness, or return of previous symptoms.
Results You Can Expect
Why Choose The Brain and Spine Centre
Cost of Hydrocephalus Treatment
Frequently Asked Questions (FAQs)
Can I know Dr. Muhammad Aqeel Natt’s credentials?
What types of brain tumours do you treat?
Is the surgery safe?
Do I need long-term follow-up after surgery?
Are you having health problems? Contact us today!
Address Business
Contact With Us
Call Us 24/7: 0318 4065914
Working Time
Sunday: 8.30am - 19.30pm

