At The Brain and Spine Centre, we specialize in the diagnosis and surgical treatment of neurological and spinal disorders. Dr. Muhammad Aqeel Natt, a leading neurosurgeon in Lahore, provides advanced, safe, and compassionate care for patients.

Paediatric Brain Tumours
Paediatric brain tumours are the most common solid tumours in children and require rapid, expert diagnosis and multidisciplinary treatment to protect neurological function and long‑term development. At The Brain and Spine Centre, Dr. Muhammad Aqeel Natt provides comprehensive care for children with brain tumours at Farooq Hospital, West Wood Branch, Lahore, including advanced neuroimaging, microsurgery, and coordination with paediatric oncology and radiotherapy teams.
Our goal is simple: safely remove or control the tumour, relieve pressure on the brain, and support the child’s growth, learning, and quality of life.
What Are Paediatric Brain Tumours?
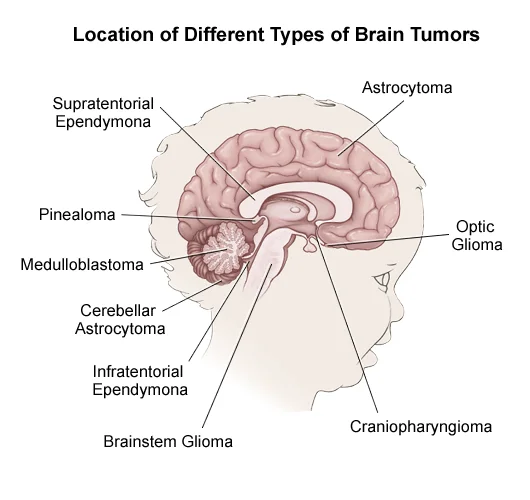
Paediatric brain tumours are abnormal growths of cells within the brain or central nervous system that can be benign (non‑cancerous) or malignant (cancerous). Their behaviour, location, and response to treatment differ significantly from adult tumours. Common tumour types in children include:
Medulloblastoma: malignant embryonal tumour of the cerebellum; often presents with hydrocephalus and ataxia.
Pilocytic astrocytoma: usually benign, slow‑growing glioma, often in cerebellum or optic pathways; frequently curable with surgery alone.
Ependymoma: arises from ependymal cells lining ventricles; may block CSF flow causing hydrocephalus.
Diffuse midline glioma / brainstem glioma: infiltrative tumours of pons or midline structures, often not amenable to complete resection.
Craniopharyngioma: benign but locally aggressive tumour near pituitary, causing endocrine and visual problems.
Tumour location (cerebrum, cerebellum, brainstem, suprasellar/pituitary region) drives symptom pattern and treatment strategy.
Symptoms of Paediatric Brain Tumours
Symptoms depend on tumour size, growth rate, and location, and may be subtle early on.
Common symptoms:
Persistent or recurrent headaches, often worse in the morning or with coughing/straining.
Nausea and vomiting, especially morning vomiting without clear GI cause.
Balance problems, clumsiness, or unsteady gait (ataxia), especially in cerebellar/posterior fossa tumours.
Visual changes: double vision, squinting, abnormal eye movements, or loss of visual fields.
Seizures in a child with no seizure history.
Behaviour, mood, or personality changes; irritability, lethargy, or sleepiness.
Weakness, numbness, or paralysis of a face, arm, or leg, often on one side.
Enlargement of head size or bulging fontanel in infants.
Any progressive combination of these symptoms warrants urgent neuroimaging.
Diagnosis
Early and accurate diagnosis relies on imaging and histology.
MRI is the preferred imaging modality, providing excellent soft‑tissue contrast to define tumour type, location, extent, and relation to eloquent brain areas. Standard protocols include T1, T2, FLAIR, diffusion, and post‑contrast sequences.
CT is often used initially in emergency settings to detect mass effect, hydrocephalus, haemorrhage, or calcifications, but MRI is needed for full characterisation.
Advanced imaging (MR spectroscopy, functional MRI, diffusion tensor imaging) may guide surgical planning near critical cortex or white matter tracts.
Surgery or stereotactic biopsy usually provides tissue for histological and molecular diagnosis, which then guides definitive therapy.
Treatment Options
Treatment is individualised based on tumour type, location, grade, spread, and age.
Surgery:
Aim is maximal safe resection while preserving neurological function.
Some tumours (e.g. pilocytic astrocytoma) may be cured with complete resection alone.
In others (e.g. medulloblastoma, ependymoma, high‑grade glioma), debulking plus adjuvant therapy is standard.
Radiation therapy:
Essential for many malignant tumours (medulloblastoma, ependymoma, high‑grade glioma, brainstem glioma) after surgery.
Techniques include conformal radiotherapy, intensity‑modulated radiotherapy (IMRT), stereotactic radiosurgery (SRS), and proton beam therapy to spare healthy tissues.
In very young children, radiation is delayed or reduced where possible to limit neurocognitive and endocrine late effects; chemotherapy is often used to defer or minimise radiation.
Chemotherapy and targeted therapy:
Used in combination with surgery and radiation for embryonal tumours, high‑grade gliomas, and ependymomas, and as primary treatment in some low‑grade gliomas where complete resection is not possible.
High‑risk protocols may include high‑dose chemotherapy with stem cell rescue in infants.
Observation:
Selected small, asymptomatic low‑grade tumours may be monitored with regular MRI scans and clinical follow‑up.
The Procedure
At The Brain and Spine Centre:
Preoperative planning: high‑resolution MRI ± tractography and functional MRI determine safest surgical route and extent of resection.
Microsurgical tumour resection: using neuronavigation, operating microscope, and intraoperative neuromonitoring to maximise tumour removal while protecting motor, language, visual and brainstem functions.
CSF diversion: many posterior fossa tumours require pre‑ or postoperative management of hydrocephalus with EVD, VP shunt, or ETV.
Multidisciplinary tumour board: neurosurgery, paediatric oncology, radiation oncology, neuroradiology, pathology, rehabilitation, and endocrinology collaborate on the optimal treatment plan.
Recovery & Aftercare
Recovery is a long‑term process, extending beyond initial hospitalisation.
Immediate postoperative period: ICU or high‑dependency care for monitoring of neurological status, CSF circulation, and complications such as oedema or haemorrhage.
Adjuvant therapy: radiotherapy and/or chemotherapy usually start after surgical recovery, following tumour‑specific protocols.
Rehabilitation: physiotherapy, occupational therapy, speech and cognitive rehabilitation address motor deficits, coordination, speech, learning, and behaviour.
Long-term follow‑up: regular MRI scans and clinic visits monitor for recurrence, late effects of treatment (endocrine, cognitive, auditory, visual), and school performance.
Results You Can Expect
Outcomes vary widely by tumour type, location, molecular profile, and response to therapy.
Survival rates exceed 80–90% for many low‑grade gliomas and some ependymomas with optimal surgery and radiotherapy.
For medulloblastoma, risk‑adapted therapy now achieves long‑term survival rates above 70–80% in standard‑risk groups, though late effects remain a concern.
Brainstem gliomas and aggressive embryonal tumours carry poorer prognosis, but clinical trials and novel therapies continue to improve outcomes.
Many survivors experience long‑term neurocognitive, endocrine, hearing, and psychosocial effects; structured survivorship care and early interventions significantly improve quality of life.
Why Choose The Brain and Spine Centre
Led by Dr. Muhammad Aqeel Natt, experienced in paediatric neuro‑oncology surgery including posterior fossa tumours, supratentorial gliomas, and midline lesions. Access to MRI‑based planning, neuronavigation and microsurgical technology for maximal safe resection. Close collaboration with paediatric oncology and radiotherapy teams to deliver protocol‑based chemotherapy and advanced radiotherapy, including conformal and stereotactic techniques where available. Long‑term multidisciplinary follow‑up with rehabilitation, neuropsychology, and endocrine support.
Cost of Paediatric Brain Tumour Treatment
Costs depend on imaging, type and number of surgeries, ICU stay, radiotherapy course, chemotherapy protocol, and long‑term rehabilitation and surveillance. Detailed, individualised estimates are provided after full diagnostic workup.
Frequently Asked Questions (FAQs)
Can I know Dr. Muhammad Aqeel Natt’s credentials?
What types of brain tumours do you treat?
Is the surgery safe?
Do I need long-term follow-up after surgery?
Are you having health problems? Contact us today!
Address Business
Contact With Us
Call Us 24/7: 0318 4065914
Working Time
Sunday: 8.30am - 19.30pm

