At The Brain and Spine Centre, we specialize in the diagnosis and surgical treatment of neurological and spinal disorders. Dr. Muhammad Aqeel Natt, a leading neurosurgeon in Lahore, provides advanced, safe, and compassionate care for patients.

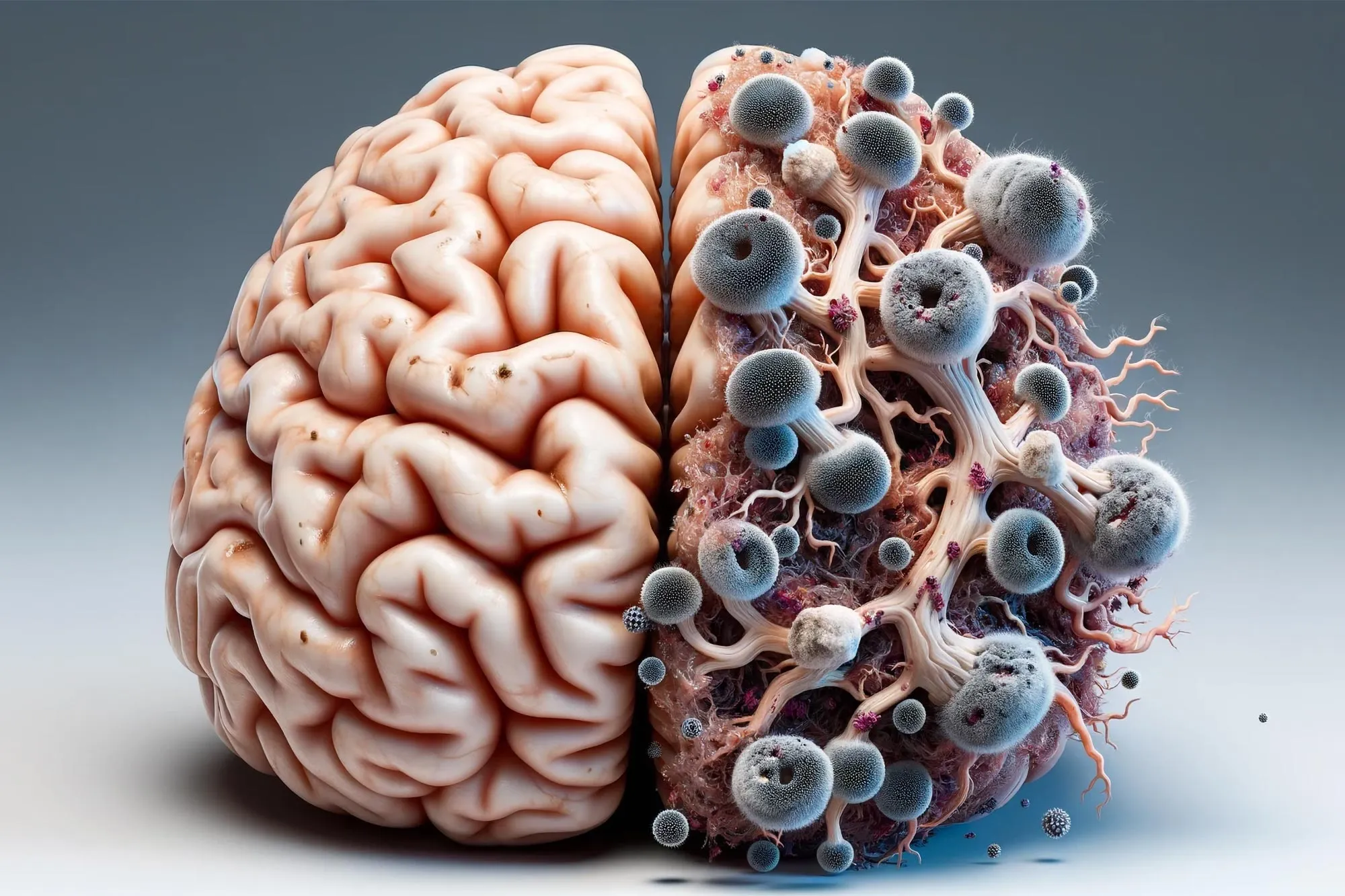
Fungal Disease
Fungal infections of the brain and central nervous system (CNS) are rare but often severe infections that require rapid diagnosis and prolonged antifungal therapy, sometimes combined with neurosurgical intervention. At The Brain and Spine Centre, Dr. Muhammad Aqeel Natt manages CNS fungal disease at Farooq Hospital, West Wood Branch, Lahore, in close collaboration with infectious disease specialists, using advanced MRI/CT imaging, targeted antifungals, and surgery where indicated.
Our goal is simple: identify the fungal infection early, control and clear it with appropriate antifungals, relieve mass effect when needed, and prevent permanent neurological damage.
What Is Fungal Disease of the Brain?
Fungal CNS disease includes meningitis, encephalitis, brain abscess, and granulomatous or mass‑like lesions caused by pathogenic or opportunistic fungi reaching the brain or meninges.
Common pathogens:
Yeasts: Cryptococcus (C. neoformans, C. gattii), Candida species.
Moulds: Aspergillus, Mucorales (mucormycosis), dematiaceous fungi.
Dimorphic fungi: Histoplasma, Coccidioides, Blastomyces in endemic areas.
Routes of spread:
Hematogenous dissemination from lungs, sinuses, skin, or bloodstream.
Direct extension from paranasal sinuses or skull base (e.g., rhinocerebral mucormycosis).
Iatrogenic/ post‑neurosurgical infections (e.g., Candida ventriculitis).
Most patients have an underlying risk factor such as HIV/AIDS, chronic steroid use, chemotherapy, transplant, uncontrolled diabetes, or recent neurosurgery.
Symptoms of Brain Fungal Disease
Symptoms usually evolve subacutely over days to weeks.
Common manifestations:
Fungal meningitis:
Headache, fever, neck stiffness, nausea, vomiting, photophobia, confusion or altered mental status.
Symptoms may appear gradually, not as abruptly as bacterial meningitis.
Parenchymal infection/abscess or granuloma:
Focal neurological deficits (weakness, numbness, speech or visual changes), seizures, personality change, or signs of raised intracranial pressure (headache, vomiting, drowsiness).
Aspergillus brain invasion can present with seizures, focal deficits, or meningitis.
Rhinocerebral mucormycosis (sinus → brain):
Facial or sinus pain, nasal congestion, dark eschar in nasal cavity, eye swelling or proptosis, headache, mental status changes.
Any meningitis‑like or focal neurological symptoms in an immunocompromised patient or following neurosurgery should raise suspicion for fungal CNS disease.
Diagnosis
Diagnosis requires a combination of imaging, CSF analysis, and microbiologic/histologic confirmation.
Imaging:
MRI with and without contrast is the modality of choice; fungal lesions can appear as ring‑enhancing abscesses, granulomas, or infiltrative masses; patterns may mimic tumours, making biopsy crucial.
Fungal abscesses often show T1 hypointense and T2 hyperintense cores with variable rim characteristics; some mould abscesses may not show classic diffusion restriction, and imaging can be misleadingly neoplastic.
CT demonstrates mass effect, hydrocephalus, haemorrhage, and sinus disease; useful in acute or unstable patients.
CSF and laboratory tests (for meningitis/ventriculitis):
Opening pressure, cell count, protein, glucose; India ink and cryptococcal antigen for Cryptococcus; culture and PCR for fungi.
CSF and blood cultures are especially important in post‑neurosurgical Candida infections.
Biopsy:
Stereotactic or open biopsy/aspiration of mass lesions often required for definitive diagnosis and to differentiate from tumour
Treatment Options
Management is urgent, prolonged, and tailored to pathogen and host status.
Antifungal therapy:
For fungal meningitis and most CNS fungal infections, initial therapy often includes amphotericin B (sometimes liposomal) plus flucytosine for induction, followed by oral azoles (e.g., fluconazole) for consolidation and maintenance, particularly in cryptococcal disease.
For Candida CNS infections (notably post‑neurosurgical), amphotericin B plus flucytosine is standard, but some series show fluconazole alone can be effective with a favourable safety profile and low relapse if used long enough.
For Aspergillus CNS infection, voriconazole is usually first‑line, sometimes combined with amphotericin B or echinocandins depending on severity and resistance patterns.
For mucormycosis, high‑dose liposomal amphotericin B is standard, with posaconazole or isavuconazole as alternatives or step‑down therapy; control of underlying risk (e.g., diabetic ketoacidosis) and aggressive surgical debridement are critical.
Duration is typically many weeks to months, guided by clinical response, imaging, and immune status.
Neurosurgical management:
Needed for:
Large mass lesions causing mass effect/raised ICP.
Diagnostic uncertainty (biopsy).
Debridement of necrotic tissue or drainage of abscesses.
Management of hydrocephalus (EVD/VP shunt) or fungal aneurysms.
Procedures include stereotactic aspiration, craniotomy/excision, shunt surgery, and repair of mycotic aneurysms.
The Procedure
Recovery & Aftercare
Recovery can be prolonged; many patients require weeks of inpatient care followed by outpatient IV or oral antifungals.
Serial MRI/CT monitors lesion size, resolution, and potential complications.
Underlying conditions (HIV, diabetes, malignancy, immunosuppression) must be optimally managed to reduce relapse and mortality.
Rehabilitation may be needed for residual neurological deficits (e.g., hemiparesis, cognitive changes, visual loss).
Results You Can Expect
Outcomes depend heavily on pathogen, immune status, lesion burden, and timing of treatment.
CNS fungal infections historically had very high mortality (e.g., 85–100% reported for some mould abscesses) but outcomes are improving with modern imaging, antifungals, and surgical care.
Early diagnosis and appropriate antifungal therapy significantly improve survival and neurological outcome, particularly in post‑neurosurgical Candida CNS infection where cure without relapse was achieved in most patients treated promptly with fluconazole in one series.
Delayed diagnosis, severe immunosuppression, multiple or deep lesions, and invasive mould infections still carry a guarded prognosis.
Why Choose The Brain and Spine Centre
Led by Dr. Muhammad Aqeel Natt, with experience in managing complex CNS infections, including fungal mass lesions and post‑neurosurgical fungal meningitis. Access to high‑quality MRI/CT and stereotactic systems to differentiate fungal lesions from tumours and guide safe biopsy. Close collaboration with infectious disease, ENT, ophthalmology, and critical care for comprehensive medical and surgical management. Individualised long‑term follow‑up addressing antifungal duration, imaging surveillance, and rehabilitation.
Cost of Fungal Brain Disease Treatment
Costs vary widely depending on length of ICU/hospital stay, type and duration of antifungals (often expensive), need for multiple surgeries, and rehabilitation. Detailed estimates are provided after a full clinical and imaging assessment.
Frequently Asked Questions (FAQs)
Can I know Dr. Muhammad Aqeel Natt’s credentials?
What types of brain tumours do you treat?
Is the surgery safe?
Do I need long-term follow-up after surgery?
Are you having health problems? Contact us today!
Address Business
Contact With Us
Call Us 24/7: 0318 4065914
Working Time
Sunday: 8.30am - 19.30pm

