At The Brain and Spine Centre, we specialize in the diagnosis and surgical treatment of neurological and spinal disorders. Dr. Muhammad Aqeel Natt, a leading neurosurgeon in Lahore, provides advanced, safe, and compassionate care for patients.

Endoscopic Third Ventriculostomy
Endoscopic third ventriculostomy (ETV) is a minimally invasive procedure that treats certain types of hydrocephalus by creating a new pathway for cerebrospinal fluid (CSF) to leave the brain, avoiding a permanent shunt. At The Brain and Spine Centre, Dr. Muhammad Aqeel Natt offers ETV at Farooq Hospital, West Wood Branch, Lahore, using modern neuroendoscopic techniques to provide durable, shunt‑free control of obstructive hydrocephalus in carefully selected children and adults.pmc.ncbi.nlm.nih+6
Our goal is simple: restore normal CSF circulation, reduce brain pressure, and minimize lifelong shunt dependence.
What Is Endoscopic Third Ventriculostomy?
ETV is an endoscopic neurosurgical procedure in which a small opening (stoma) is made in the floor of the third ventricle, allowing CSF to bypass a blockage (such as aqueductal stenosis or tumor obstruction) and flow directly into the basal cisterns and subarachnoid spaces. Unlike ventriculoperitoneal (VP) shunts, ETV does not leave permanent hardware in the body and therefore avoids many long‑term shunt-related complications.
ETV is most effective in obstructive (non‑communicating) hydrocephalus, including:
Aqueductal stenosis
Posterior fossa tumours compressing the aqueduct or fourth ventricle outlets
Some cases of shunt failure with occlusive hydrocephalus
Success is lower in post‑infectious and post‑haemorrhagic communicating hydrocephalus, especially in young infants.
Symptoms and Indications
ETV is considered when hydrocephalus causes symptoms and imaging shows an obstructive pattern.
Typical indications:
Symptomatic aqueductal stenosis with enlarged lateral and third ventricles but small fourth ventricle.
Tumour‑related obstructive hydrocephalus (e.g. tectal glioma, pineal or posterior fossa masses) where CSF pathways are blocked.
Selected patients with shunt malfunction and occlusive hydrocephalus who may benefit from shunt independence.
Certain cases of normal pressure or chronic obstructive hydrocephalus in adults where ETV has shown good long-term results.
Patients typically have:
Headache, nausea, vomiting, papilledema, lethargy, or visual changes from raised intracranial pressure.
Gait disturbance, cognitive decline, or urinary incontinence in chronic adult hydrocephalus.
Diagnosis
Diagnosis confirms hydrocephalus type and suitability for ETV.
MRI with sagittal T2 and CSF flow studies is ideal; it shows ventricular enlargement, aqueduct or outflow obstruction, and helps predict ETV success. A postoperative “flow void” at the stoma correlates strongly with clinical success.
CT scan quickly confirms ventriculomegaly and obstructive pattern, but MRI better visualizes floor anatomy and cisterns.
ETV Success Score (ETVSS) may be used to estimate the probability of success based on age, aetiology, and prior shunting.
The Procedure
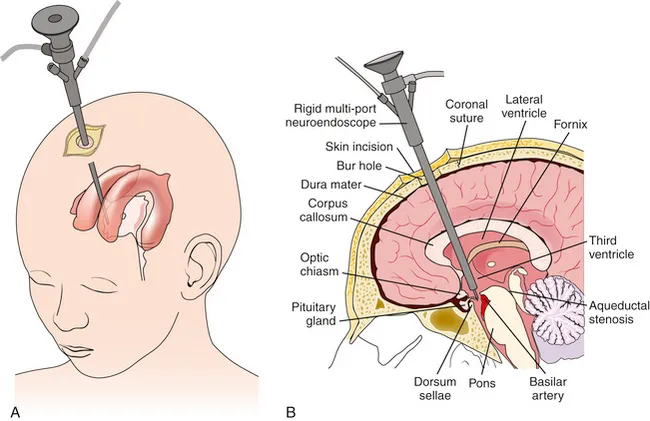
ETV is performed under general anaesthesia using a rigid neuroendoscope.
Key steps:
A small burr hole is made in the frontal skull, usually just anterior to the coronal suture.
The endoscope is passed through the lateral ventricle into the third ventricle under direct vision.
The floor of the third ventricle (between the infundibular recess and mammillary bodies) is carefully perforated with a blunt instrument or balloon catheter, creating a stoma that opens into the prepontine cistern.
The opening is enlarged and inspected to ensure CSF can circulate freely and no critical vessels are injured.
The endoscope is withdrawn and the wound closed; no shunt hardware is left in place.
Operative time is usually short (often under 1 hour), and blood loss is minimal in experienced hands.
Recovery & Aftercare
Recovery is generally faster and simpler than with shunt surgery.
Most patients spend 1–3 days in hospital for observation.
Symptoms of raised intracranial pressure (headache, vomiting) typically improve within days if ETV is successful.
Follow‑up MRI assesses ventricular size and confirms CSF flow through the stoma; persistent flow void is strongly associated with durable clinical improvement.
Families are educated about signs of ETV failure: recurrence of headache, vomiting, drowsiness, visual changes, or other hydrocephalus symptoms requiring urgent reassessment.
Results You Can Expect
ETV has good success rates and a favourable safety profile in well‑selected patients.
Large adult series report overall success rates around 74–76%, with higher rates (up to 83–95%) in aqueductal stenosis and tumour‑related hydrocephalus.
In mixed‑age cohorts, success rates commonly fall between 70–85%, with minimal morbidity and no mortality in many series.
Local and regional studies show success rates of 73.3–79.4% with low complication rates, confirming ETV as a reliable alternative to VP shunt in obstructive hydrocephalus.
In infants <1 year, success is more modest (e.g. ~57% in one infant series), but complication rates remain lower than with shunts, supporting ETV as a reasonable option in selected obstructive cases.
Complication profile:
Overall complication rates range from about 9–23%, mostly minor and transient, including CSF leak, fever, minor haemorrhage, or subdural collections.
Serious complications such as arterial injury, hypothalamic or thalamic damage, or permanent neurological deficit are rare in experienced hands.
Compared with VP shunts, ETV has fewer long‑term mechanical failures and infections, although shunts may be more effective initially in some severe or communicating hydrocephalus cases.
Why Choose The Brain and Spine Centre
Led by Dr. Muhammad Aqeel Natt, experienced in neuroendoscopy and CSF diversion procedures (ETV, ETV‑CPC, and shunt surgery). Careful preoperative selection using MRI‑based assessment and established ETV success criteria to optimise outcomes and avoid unnecessary procedures. State‑of‑the‑art endoscopic equipment and techniques to minimise complications and maximise long‑term shunt independence. Integrated hydrocephalus program coordinating imaging, intraoperative decision‑making, and long‑term follow‑up for both children and adults.
Cost of Endoscopic Third Ventriculostomy
Costs depend on imaging (MRI/CT), operative time and equipment, length of hospital stay, and any adjunct procedures (e.g. ETV‑CPC, tumour biopsy). ETV is generally more cost‑effective over time than VP shunts due to fewer revisions and hardware complications. A personalised cost estimate is provided after consultation and imaging review.
Frequently Asked Questions (FAQs)
Can I know Dr. Muhammad Aqeel Natt’s credentials?
What types of brain tumours do you treat?
Is the surgery safe?
Do I need long-term follow-up after surgery?
Are you having health problems? Contact us today!
Address Business
Contact With Us
Call Us 24/7: 0318 4065914
Working Time
Sunday: 8.30am - 19.30pm

