At The Brain and Spine Centre, we specialize in the diagnosis and surgical treatment of neurological and spinal disorders. Dr. Muhammad Aqeel Natt, a leading neurosurgeon in Lahore, provides advanced, safe, and compassionate care for patients.

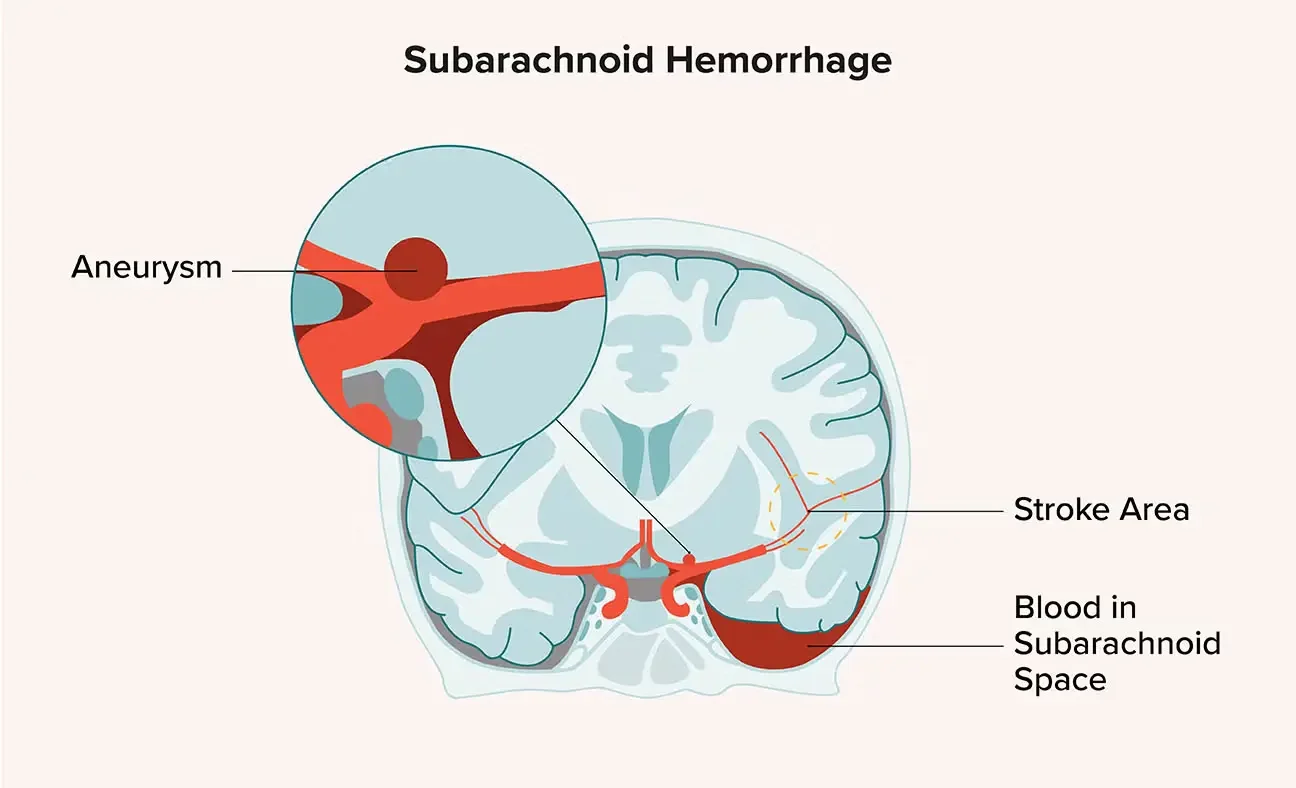
Subarachnoid Hemorrhage
Subarachnoid hemorrhage is a neurosurgical emergency involving bleeding into the space between the brain and the membranes covering it, most commonly from rupture of a cerebral aneurysm, and carries high risk of death and disability if not promptly identified and treated. At The Brain and Spine Centre, Dr. Muhammad Aqeel Natt provides urgent neurosurgical and neuro-intensive care for SAH at Farooq Hospital, West Wood Branch, Lahore, including rapid imaging, early aneurysm repair by clipping or coiling, and comprehensive management of complications.
Our goal is simple: identify and secure the bleeding source, prevent rebleeding, manage complications, and minimize neurological damage and death.
What Is Subarachnoid Hemorrhage?
Subarachnoid hemorrhage is acute bleeding into the subarachnoid space—the area between the brain surface and the arachnoid membrane. The bleeding causes acute elevations in intracranial pressure, chemical meningitis, secondary vasospasm with brain ischemia, and often hydrocephalus.
Causes:
Ruptured cerebral aneurysm: accounts for ~85% of spontaneous (non-traumatic) cases. Aneurysms are typically located in the circle of Willis and are classified as berry (saccular) aneurysms.
Arteriovenous malformations (AVMs): abnormal tangles of vessels prone to bleeding.
Traumatic SAH: from head injury, particularly in younger patients.
Other causes: vasculitis, coagulopathy, anticoagulant use, sympathomimetic drugs (cocaine), mycotic aneurysms from endocarditis.
Symptoms of Subarachnoid Hemorrhage
SAH presents with distinctive, sudden-onset features.
Classic presentation:
Sudden, severe “thunderclap” headache, often described as the “worst headache of my life,” starting in a fraction of a second and becoming maximally severe almost immediately.
Nausea, vomiting, and stiff neck.
Brief loss of consciousness, followed by confusion, drowsiness, or prolonged coma in severe cases.
Focal neurological deficits (weakness, paralysis, speech changes, vision problems, pupil changes, cranial nerve palsies) in ~25% of patients, often from mass effect of blood or associated aneurysm.
Seizures.
Fluctuating heart rate and blood pressure.
Sentinel headache: some patients experience a smaller “warning” leak or sentinel bleed minutes to weeks before the major rupture.
Diagnosis
Common causes include:
- Long-standing high blood pressure (hypertension) damaging small brain arteries, the leading cause of spontaneous ICH
- Ruptured intracranial aneurysm causing subarachnoid hemorrhage
- Arteriovenous malformations (AVMs) and other vascular malformations
- Cerebral amyloid angiopathy (CAA), especially in older adults, causing lobar hemorrhages and microbleeds
- Head trauma
- Overtreatment with blood thinners (anticoagulants) and antiplatelet drugs
- Less commonly, tumors, vasculitis, or bleeding disorders
Major risk factors include uncontrolled hypertension, smoking, heavy alcohol use, older age, and previous stroke or hemorrhage.
Treatment Options
Neurosurgical and endovascular treatments aim to secure the aneurysm and prevent rebleeding.
Aneurysm securing (primary goal):
Two main modalities are used, often selected based on aneurysm anatomy, patient age/health, and institutional expertise.
Microsurgical clipping:
Craniotomy approach under general anaesthesia; the aneurysm neck is clipped with a titanium clip to exclude it from circulation.
Advantages: complete, durable occlusion; lower rebleeding rate (~48% reduction vs coiling).
Disadvantages: more invasive; greater inflammatory response and potentially higher early poor outcomes; longer operative time and hospitalisation.
Endovascular coiling:
Catheter-based approach under local or general anaesthesia; detachable coils fill the aneurysm, inducing thrombosis.
Advantages: minimally invasive; faster recovery; better functional outcomes at discharge and 1-year follow-up.
Disadvantages: incomplete occlusion risk (~48% higher rebleeding risk vs clipping); may require repeat treatment; coils can compact over time.
Current evidence: Meta-analysis shows clipping has superior durability and lower rebleeding risk, but coiling yields better functional outcomes and faster recovery; choice depends on aneurysm anatomy, patient condition, and institutional expertise.
Supportive and preventive care:
Strict blood pressure and ICP management to prevent rebleeding.
Management of secondary vasospasm (peak days 4–10) with calcium channel blockers (e.g., nimodipine) and, if needed, transluminal angioplasty or intra-arterial vasodilators.
Prevention and treatment of rebleeding (highest risk in first 7 days), seizures, hydrocephalus (may require EVD/VP shunt), hyponatraemia, and other medical complications.
The Procedure
At The Brain and Spine Centre:
Emergency stabilisation: rapid airway management, ICU-level monitoring, venous access, and blood pressure control.
Rapid imaging and decision-making: emergency CT/CTA or DSA to diagnose and plan aneurysm treatment.
Urgent aneurysm repair:
Clipping via microsurgical craniotomy or endovascular coiling via catheter-based approach, depending on aneurysm anatomy and patient status.
Goal is treatment within 24 hours or as soon as safely feasible; delays >3 days are associated with increased poor outcomes.
Neuro-ICU care: continuous monitoring, vasospasm prevention/management, seizure prophylaxis, CSF diversion if hydrocephalus develops, and management of complications.
Recovery & Aftercare
ICU stay typically 7–14 days or longer, depending on severity and complications.
Neurological recovery can continue over weeks to months; many survivors experience residual cognitive, emotional, or motor deficits.
Vasospasm monitoring and management are critical during the high-risk window (days 4–10).
Long-term follow-up includes repeat imaging, cognitive/neuropsychological assessments, rehabilitation, and screening for recurrent aneurysms or familial disease.
Results You Can Expect
Outcomes depend on initial severity (Hunt–Hess or WFNS grade), aneurysm location/size, time to treatment, and complications.
Mortality for aneurysmal SAH is significant: ~10–15% die before reaching hospital; in-hospital mortality is ~10–20% with modern treatment.
Of survivors, many achieve good functional recovery with proper care; about 50–60% have good neurological outcomes with either clipping or coiling.
Rebleeding risk without treatment is ~20% in first 2 weeks; securing the aneurysm reduces this dramatically.
Why Choose The Brain and Spine Centre
Led by Dr. Muhammad Aqeel Natt, with expertise in both microsurgical aneurysm clipping and coordination with endovascular colleagues for coiling. Rapid 24/7 neurosurgical response with access to emergency CT/CTA and operating theatre capacity. Comprehensive neuro-ICU management of vasospasm, hydrocephalus, rebleeding prevention, and other SAH complications. Evidence-based aneurysm repair selection and aggressive vasospasm prevention to maximise functional recovery.
Cost of Subarachnoid Hemorrhage Treatment
Costs are substantial and include emergency imaging, ICU stay (often 1–2 weeks), craniotomy/endovascular procedure, medications, and rehabilitation. Emergency cases are managed regardless of financial constraints. Detailed cost discussions occur when clinically feasible.
Frequently Asked Questions (FAQs)
Can I know Dr. Muhammad Aqeel Natt’s credentials?
What types of brain tumours do you treat?
Is the surgery safe?
Do I need long-term follow-up after surgery?
Are you having health problems? Contact us today!
Address Business
Contact With Us
Call Us 24/7: 0318 4065914
Working Time
Sunday: 8.30am - 19.30pm

