At The Brain and Spine Centre, we specialize in the diagnosis and surgical treatment of neurological and spinal disorders. Dr. Muhammad Aqeel Natt, a leading neurosurgeon in Lahore, provides advanced, safe, and compassionate care for patients.

NPH (Normal Pressure Hydrocephalus)
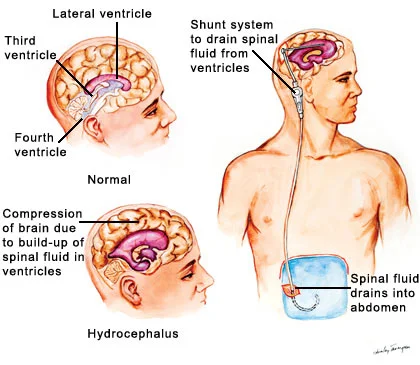
Normal pressure hydrocephalus is a neurosurgical disorder characterized by the clinical triad of gait disturbance (“magnetic gait”), cognitive decline, and urinary incontinence caused by impaired cerebrospinal fluid (CSF) absorption, resulting in ventricular enlargement despite normal opening pressures on lumbar puncture. At The Brain and Spine Centre, Dr. Muhammad Aqeel Natt diagnoses and treats NPH at Farooq Hospital, West Wood Branch, Lahore, using advanced neuroimaging, CSF dynamics assessment, and ventriculoperitoneal (VP) shunt placement to restore cognitive and motor function.
Our goal is simple: identify NPH early, confirm CSF dynamics abnormality, and place a shunt to restore gait, cognition, and continence before irreversible neuronal loss occurs.
What Is Normal Pressure Hydrocephalus?
Normal pressure hydrocephalus is a communicating hydrocephalus in which impaired CSF absorption at the arachnoid granulations leads to progressive ventricular enlargement (ventriculomegaly) despite normal CSF opening pressure (<25 cm H₂O) and normal CSF composition. Pathophysiology involves reduced CSF compliance, increased brain water content, and altered cerebral blood flow; the mechanism is not fully understood.
Idiopathic NPH (iNPH): most common (~90%); occurs without preceding illness.
Secondary NPH: follows subarachnoid hemorrhage, meningitis, head trauma, or spinal cord injury (~10%).
Symptoms of Normal Pressure Hydrocephalus
Classic presentation includes the triad, though not all three need be present for diagnosis.
Gait disturbance (90-100% of cases):
Characteristic “magnetic gait”—wide-based, shuffling, slow; feet appear to stick to floor (“magnetic attraction”); difficulty initiating steps.
Mild balance impairment, propulsive gait, or falls in advanced disease.
Asymmetric involvement in some cases.
Cognitive decline (60-90% of cases):
Bradykinesia (slowed thinking), reduced verbal fluency, poor executive function, memory loss (subcortical pattern).
Apathy, reduced initiation; depression common.
Usually precedes or accompanies gait changes; ranges mild to severe dementia.
Urinary incontinence (50-70% of cases):
Urgency and frequency, then frank incontinence (late).
Often attributed to aging or prostate disease initially; key clue is isolated urgency without detrusor overactivity on urodynamics.
Additional features:
Onset insidious over months-years; often mistaken for Parkinson’s disease, Alzheimer’s, or Lewy body dementia.
Early-stage NPH may present with isolated gait slowing or cognitive complaint.
Diagnosis
Diagnosis integrates clinical, neuroimaging, and CSF dynamics findings.
Clinical criteria (Marmarou):
Gait disturbance ≥2 months + cognitive decline (Folstein <24) or urinary dysfunction.
Neuroimaging (MRI gold standard):
Ventriculomegaly: Evans’ index >0.3 (ventricular width/brain width at lateral ventricles)
Disproportionate enlargement of lateral/third ventricles relative to sulci (normal-pressure signature: enlargement despite normal/mild cortical atrophy)
T2-FLAIR hyperintensity along lateral ventricles (transependymal CSF flow)
No Chiari malformation, syrinx, or tethering.
CSF dynamics assessment:
Tap test (lumbar puncture with needle in situ): withdraw 30-50 ml CSF; assess gait/cognition over 1-2 hours immediately post-LP and next day.
Positive tap test (improvement in gait/cognition) strongly predicts shunt response; negative test does not exclude NPH.
Intracranial pressure monitoring (24-hour ICP): intermittent pressure waves (B-waves, plateau waves) in some NPH patients; not standard of care.
Lumbar infusion test: measures CSF outflow resistance; low outflow resistance (<13 mmHg/ml/min) suggests NPH.
Treatment Options
Conservative management:
Acetazolamide, thiazide diuretics: reduce CSF production; modest benefit (20-30% improvement) in some early-stage cases.
PT/gait training: supportive but not curative.
Surgical management (VP shunt):
Indications: clinical triad + ventriculomegaly + positive tap test or imaging/CSF dynamics consistent with NPH; shunt response >50% likely.
Contraindications: cortical dementia (Alzheimer’s pathology), absence of gait/cognitive changes, very advanced disease, significant cortical atrophy, significant comorbidities precluding surgery.
VP shunt: silicone catheter from lateral ventricle to peritoneal cavity; includes programmable valve, anti-siphon device; diverts excess CSF, reducing ventricular pressure/size.
The Procedure
Performed under general anaesthesia; 1-2 hours.
Key steps:
Patient supine or lateral decubitus position.
Frontal or parietal burr hole for ventricular catheter placement; often right side.
Ultrasound or landmark-guided catheter tunneling to lateral ventricle; CSF flow confirms placement.
Subcutaneous tunnel created from head to neck to abdomen.
Peritoneal catheter placed via small laparotomy or percutaneous trocar; catheter confirmed free in peritoneal cavity.
Valve system (programmable, anti-siphon) connects catheters; set to opening pressure (typically 150-200 mmH₂O initially).
Closure and postoperative imaging (X-ray shunt series or CT to confirm positioning).
Recovery & Aftercare
Hospital stay: 3-7 days; gradual mobilization postoperative day 1.
Head bandage; avoid strenuous activity 4 weeks.
Follow-up X-ray shunt series (head, chest, abdomen) at 2-4 weeks to confirm catheter position.
Clinical reassessment: gait, cognition, continence; most improvement noted 2-6 weeks, but can continue 3-12 months.
Valve adjustment (programming) if needed based on clinical response; programmable valves allow non-invasive pressure modulation.
Lifelong surveillance: shunt function monitored; replacement/revision required if malfunction or infection.
Results You Can Expect
Gait improvement: 60-90% of patients experience improved walking ability, reduced falls, faster gait speed.
Cognitive improvement: 50-70% show cognitive gains; greatest benefit if symptom duration <2 years.
Continence: 50-70% regain urinary control; incontinence may be only partially reversible if long-standing.
Overall functional improvement: 70-80% achieve meaningful benefit in ≥1 symptom domain.
Predictors of good shunt response:
Symptom duration <2-3 years (shorter duration → better prognosis).
Positive tap test.
Gait dysfunction prominent relative to dementia.
Absent severe cortical atrophy on MRI.
Complications:
Shunt malfunction (obstruction, disconnection): 5-10%/year; presents with recurrent symptoms.
Shunt infection (ventriculitis, meningitis): 1-3%; treated with antibiotics ± shunt removal/replacement.
Subdural hematoma: 2-5%; from overshunting or falls post-shunt.
Over-drainage: headaches, cortical slit ventricles; managed by valve pressure adjustment.
Why Choose The Brain and Spine Centre
Led by Dr. Muhammad Aqeel Natt, with expertise in NPH diagnosis, shunt placement, and long-term management. Access to advanced MRI (3T) for precise ventriculomegaly assessment and Evans’ index calculation. Capability to perform lumbar infusion testing for CSF dynamics confirmation if needed. Multidisciplinary evaluation: neurology, neuropsychology, neuroradiology to ensure appropriate patient selection and optimize outcomes. Programmable shunt technology allowing non-invasive adjustment for clinical optimization. 24/7 shunt malfunction emergency protocols.
Cost of Normal Pressure Hydrocephalus Treatment
Diagnostic workup (MRI, LP, tap test): moderate cost.
VP shunt surgery (device, OR, hospital stay): significant cost; varies by shunt type (programmable more expensive but adjustable vs fixed-pressure).
Long-term: shunt surveillance, programming, and replacement/revision costs.
Detailed estimates provided after imaging and clinical assessment; cost-effective given functional recovery potential.
Frequently Asked Questions (FAQs)
Can I know Dr. Muhammad Aqeel Natt’s credentials?
What types of brain tumours do you treat?
Is the surgery safe?
Do I need long-term follow-up after surgery?
Are you having health problems? Contact us today!
Address Business
Contact With Us
Call Us 24/7: 0318 4065914
Working Time
Sunday: 8.30am - 19.30pm

