At The Brain and Spine Centre, we specialize in the diagnosis and surgical treatment of neurological and spinal disorders. Dr. Muhammad Aqeel Natt, a leading neurosurgeon in Lahore, provides advanced, safe, and compassionate care for patients.

ACDF
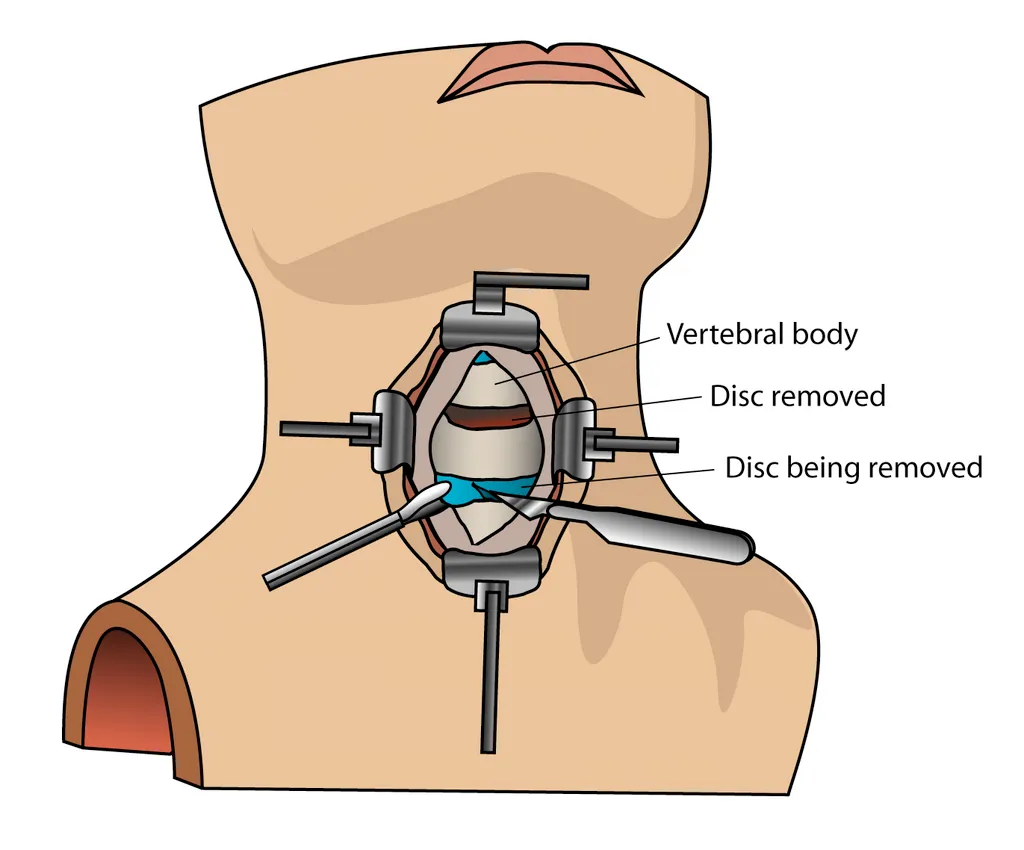
ACDF is a common neck surgery that relieves pressure on spinal nerves or the spinal cord by removing a damaged cervical disc and fusing the adjacent vertebrae. At The Brain and Spine Centre, Dr. Muhammad Aqeel Natt offers ACDF at Farooq Hospital, West Wood Branch, Lahore, using modern anterior approaches and fusion techniques to treat cervical radiculopathy and myelopathy.
Our goal is simple: decompress nerves safely, stabilize the cervical spine, and restore arm function and neck comfort.
What Is ACDF?
Anterior cervical discectomy and fusion (ACDF) is a decompression–stabilization procedure performed through the front of the neck. The surgeon removes the diseased or herniated disc (and any bone spurs) to relieve pressure on the spinal cord or nerve roots, then places a bone graft or cage and usually a plate with screws to fuse the adjacent vertebrae for long-term stability. ACDF is considered the gold-standard surgical treatment for cervical radiculopathy and myelopathy when conservative measures fail.
Symptoms and Indications
ACDF is typically recommended for:
- Cervical radiculopathy: neck pain with arm pain, numbness, tingling, or weakness due to disc herniation or foraminal stenosis.
- Cervical myelopathy: hand clumsiness, gait imbalance, leg stiffness, and long‑tract signs from spinal cord compression.
- Persistent or worsening symptoms despite adequate conservative treatment (medications, physiotherapy, injections).
- Progressive neurological deficits traced to cervical pathology (worsening weakness, sensory loss, spasticity).
- Cervical disc degeneration, spinal stenosis, or trauma-induced instability requiring anterior decompression and stabilization.
ACDF is most commonly used for 1–2 level disease and can be extended to multilevel cases when appropriate.
Diagnosis
Preoperative evaluation includes:
- Detailed history and neurological exam to document radiculopathy or myelopathy signs.
- Cervical MRI to visualize disc herniation, osteophytes, spinal cord/nerve compression, and canal/foraminal narrowing.
- X‑rays (including flexion–extension) to assess alignment, disc height, and instability.
- CT may be used to define bony anatomy and plan decompression in complex spondylosis or OPLL.
The Procedure
ACDF is performed under general anesthesia with the patient supine.
Key steps:
- A small transverse or oblique incision is made in the front of the neck, and a natural tissue plane is used to gently move aside muscles, trachea, and esophagus, exposing the cervical spine.
- The target disc is removed in its entirety (discectomy), along with any bone spurs or posterior osteophytes compressing the nerve roots or spinal cord (foraminotomy, osteophytectomy).
- The decompressed disc space is filled with a bone graft or interbody cage, restoring disc height and foraminal space.
- A small plate and screws are typically applied to secure the vertebrae while fusion occurs over the following months.
- The wound is closed in layers; most cases require only a short hospital stay.
ACDF directly addresses the source of compression and stabilizes the motion segment, making it the procedure of choice for single‑level disc disease and frequently for two‑level disease.
Recovery & Aftercare
Recovery varies with age, pre-operative myelopathy severity, and whether fusion is performed.
- Hospital stay typically ranges from 2–5 days depending on comorbidities and the extent of surgery.
- Neck soreness and stiffness are common initially and gradually improve with physiotherapy; collars may be used short-term as directed.
- Walking usually resumes early, with gait and balance improving over weeks to months as cord function recovers.
- Formal rehabilitation helps restore neck mobility (within safe limits), upper limb dexterity, and gait, and reduces long-term stiffness.
- Long-term follow-up with clinical assessment and, when indicated, MRI is important to monitor decompression, fusion status, and adjacent segment health.
- Short‑term outcomes often show significant myelopathy improvement, but long‑term results can be influenced by age, pre-operative severity, and trauma. Older patients (>70 years), those with severe preoperative myelopathy, long symptom duration (>6–18 months), or trauma history have higher risk of delayed deterioration.
Results You Can Expect
Why Choose The Brain and Spine Centre
Cost of ACDF
Costs vary with the number of levels fused, type of implants and grafts used, hospital stay, imaging, and rehabilitation needs. Personalized cost estimates are provided after consultation and imaging review.
Frequently Asked Questions (FAQs)
Can I know Dr. Muhammad Aqeel Natt’s credentials?
What types of brain tumours do you treat?
Is the surgery safe?
Do I need long-term follow-up after surgery?
Are you having health problems? Contact us today!
Address Business
Contact With Us
Call Us 24/7: 0318 4065914
Working Time
Sunday: 8.30am - 19.30pm

