At The Brain and Spine Centre, we specialize in the diagnosis and surgical treatment of neurological and spinal disorders. Dr. Muhammad Aqeel Natt, a leading neurosurgeon in Lahore, provides advanced, safe, and compassionate care for patients.

AVM Malformation Surgery
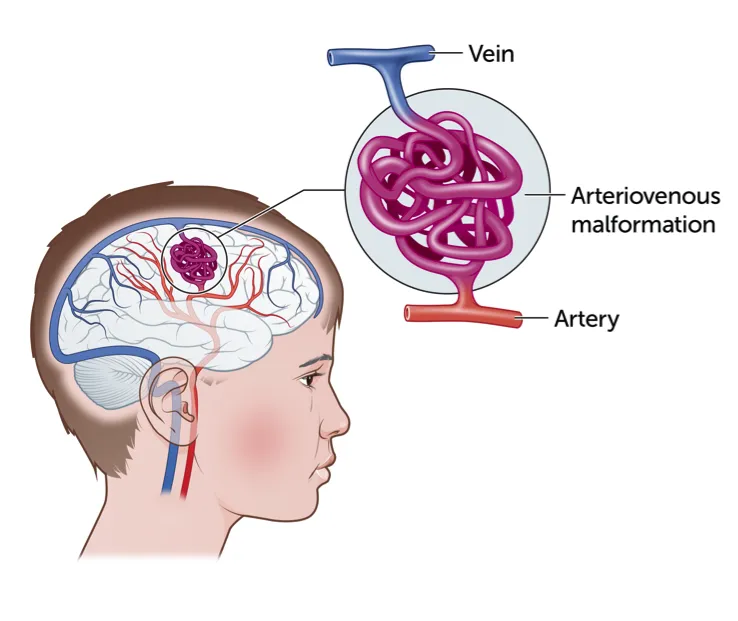
Arteriovenous malformations are complex abnormal tangles of blood vessels that bypass normal capillaries, putting the brain at risk of bleeding and neurological complications. At The Brain and Spine Centre, Dr. Muhammad Aqeel Natt provides comprehensive AVM care at Farooq Hospital, West Wood Branch, Lahore, offering expert diagnosis, multidisciplinary treatment including surgery, embolization, and radiosurgery to achieve safe, definitive cure.
Our goal is simple: obliterate the AVM safely, prevent bleeding, and preserve neurological function for the best possible quality of life.
What Is an Arteriovenous Malformation?
An arteriovenous malformation (AVM) is an abnormal, tangled web of arteries and veins in the brain where blood bypasses the normal capillary network and flows directly from high-pressure arteries into low-pressure veins. This direct shunting causes rapid, turbulent blood flow under excessive pressure, weakening vessel walls and putting the patient at risk of catastrophic brain hemorrhage. AVMs vary in size, location, and complexity; the Spetzler–Martin grading system (Grades I–V) helps stratify risk and guide treatment.
Symptoms of Arteriovenous Malformation
Many patients are asymptomatic until hemorrhage occurs; approximately 50% of AVMs first present with bleeding.
Common symptoms from AVM (unruptured or chronic):
- Headaches or persistent pain localized to one area
- Seizures, often the presenting symptom
- Muscle weakness, numbness, or paralysis in part of the body
- Vision loss, double vision, or visual field defects
- Speech or language difficulties
- Dizziness or balance problems
- Pulsatile tinnitus (hearing a pulse-like sound in the ear)
Symptoms from AVM hemorrhage (acute):
- Sudden, severe headache
- Sudden weakness, numbness, or paralysis
- Vision loss or confusion
- Difficulty walking or loss of consciousness
- Seizures
Diagnosis
Accurate diagnosis and characterization are essential for treatment planning.
Imaging modalities include:
- MRI: Sensitive for detecting AVMs and visualizing associated bleeding, edema, and exact location; MR angiography identifies feeding arteries and draining veins.
- CT scan: Rapidly detects acute bleeding; CT angiography (CTA) is highly sensitive (93.75% for AVMs <3 cm) for defining AVM morphology, eloquent brain involvement, deep venous drainage, and associated aneurysms.
- Cerebral angiography (DSA): Gold standard for detailed AVM visualization; shows precise feeding arteries, nidus structure, draining veins, and aneurysms crucial for surgical or endovascular planning.
Treatment Options
Management depends on AVM size, location (eloquent vs. non-eloquent), grade, hemorrhage history, and patient factors. A multidisciplinary approach often combines modalities.
- Observation: Small, asymptomatic, low-grade AVMs with low hemorrhage risk may be managed with serial imaging and seizure prophylaxis instead of intervention.
Microsurgical resection:
- Direct surgical excision remains the gold standard for definitive AVM eradication, especially for small, accessible, lower-grade (Grade I–II) AVMs.
- Provides immediate obliteration and eliminates future hemorrhage risk.
Endovascular embolization:
- Minimally invasive catheter-based technique using embolic agents (glue, coils, particles) to reduce blood flow into the AVM.
- Can serve as standalone therapy for select small AVMs.
- Often used to make larger AVMs surgically resectable or to reduce size before radiosurgery.
- Helps eliminate hemodynamic risk factors for hemorrhage and treats radioresistant aneurysms prior to SRS.
Stereotactic radiosurgery (SRS):
- Uses convergent radiation beams (Gamma Knife, CyberKnife, LINAC) to target the AVM nidus in single or multiple sessions.
- Ideal for small (<2.5 cm), deep, or eloquent AVMs where surgery carries high risk.
- AVM obliteration occurs gradually over 1–3 years, during which hemorrhage risk persists.
- Fractionated SRS enables treatment of larger AVMs (>2.5 cm) by dividing dosage to reduce radiation-related injury.
The Procedure
Our multidisciplinary approach tailors treatment to AVM characteristics:
- Detailed clinical, radiological, and angiographic evaluation to grade the AVM and determine the optimal management strategy (surgery, embolization, SRS, or combination).
- For surgical candidates: Microscope-guided craniotomy with meticulous nidus dissection and feeding artery ligation to achieve complete resection.
- Preoperative embolization may reduce intraoperative blood loss and facilitate complete resection.
- SRS planning: High-resolution imaging and 3D planning are used to deliver a focused radiation dose while minimizing toxicity to surrounding brain tissue.
Recovery & Aftercare
Recovery varies with treatment modality and AVM characteristics:
- Microsurgery: 1–2 week hospital stay; gradual neurological recovery over weeks to months; seizure prophylaxis continued; imaging at 6 weeks confirms obliteration.
- Embolization: Typically outpatient or 1-day stay; minimal recovery time; staged embolization sessions may be required.
- SRS: Outpatient procedure; gradual AVM obliteration over 1–3 years; serial MRI and angiography used to monitor treatment response.
- Long-term follow-up imaging confirms complete AVM obliteration and monitors for late complications such as radiation necrosis.
Results You Can Expect
Why Choose The Brain and Spine Centre
Led by Dr. Muhammad Aqeel Natt, specialist neurosurgeon with extensive expertise in microsurgical AVM resection, complex craniotomy planning, and multidisciplinary AVM management. Access to advanced MRI, CTA, and cerebral angiography for precise AVM characterization and surgical planning. Partnerships with interventional neuroradiologists for endovascular embolization and radiation oncologists for SRS to offer complete multidisciplinary care. Convenient location at Farooq Hospital, West Wood Branch, Lahore with modern operating, imaging, and SRS facilities.
Cost of AVM Treatment
Costs vary with treatment modality (surgery vs. embolization vs. SRS vs. combined), AVM grade and size, hospital stay, and follow-up imaging requirements. Personalized estimates provided after consultation and imaging review.
Frequently Asked Questions (FAQs)
Can I know Dr. Muhammad Aqeel Natt’s credentials?
What types of brain tumours do you treat?
Is the surgery safe?
Do I need long-term follow-up after surgery?
Are you having health problems? Contact us today!
Address Business
Contact With Us
Call Us 24/7: 0318 4065914
Working Time
Sunday: 8.30am - 19.30pm

