At The Brain and Spine Centre, we specialize in the diagnosis and surgical treatment of neurological and spinal disorders. Dr. Muhammad Aqeel Natt, a leading neurosurgeon in Lahore, provides advanced, safe, and compassionate care for patients.

Brachial Plexus Injuries
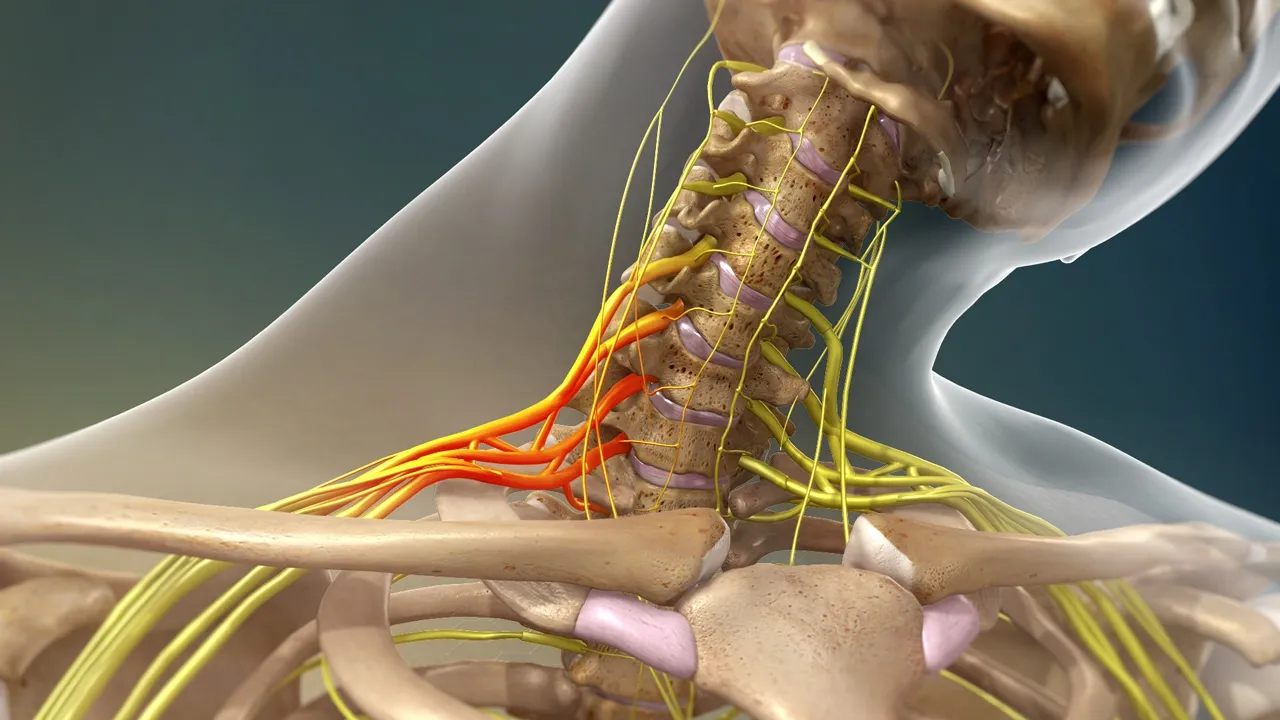
Brachial plexus injuries involve damage to the network of nerves that control movement and sensation in the shoulder, arm, and hand, and can cause pain, weakness, or even complete paralysis of the limb. At The Brain and Spine Centre, Dr. Muhammad Aqeel Natt provides comprehensive evaluation and microsurgical reconstruction of brachial plexus injuries at Farooq Hospital, West Wood Branch, Lahore, combining detailed imaging, electrodiagnostics, and advanced nerve repair and nerve transfer techniques.
Our goal is simple: accurately define the level and severity of nerve damage, restore as much arm and hand function as possible, and reduce chronic neuropathic pain.
What Are Brachial Plexus Injuries?
The brachial plexus is a complex network of spinal nerves (C5–T1) that exit the neck and branch to innervate the shoulder, arm, and hand. Brachial plexus injuries occur when these nerves are stretched, compressed, torn, or avulsed (pulled out of the spinal cord).
Common causes:
High‑energy trauma: motorcycle/car accidents, falls, industrial injuries, penetrating trauma.
Birth trauma: neonatal brachial plexus palsy during difficult delivery (Erb’s or Klumpke’s palsy).
Tumours, radiation fibrosis, or inflammation (Parsonage–Turner syndrome).
Injury patterns range from transient neuropraxia (“burners”/“stingers”) to complete root avulsions with global paralysis of the limb.
Symptoms of Brachial Plexus Injury
Symptoms depend on which roots/trunks are affected and how severely.
Common features:
Burning, stinging, or electric shock‑like pain in shoulder or arm at the time of injury (typical in sports “stingers”).
Weakness or inability to use shoulder, elbow, wrist, or hand muscles; complete paralysis in severe injuries.
Numbness or loss of sensation in the arm, forearm, or hand.
Flail limb with no movement and no sensation in complete plexus injuries.
In neonatal lesions: absent Moro reflex on one side, arm adducted and internally rotated (Erb’s palsy), or hand weakness and clawing (Klumpke’s palsy).
Types of anatomical nerve injury:
Neuropraxia (stretch): mild, conduction block without structural disruption; often recovers spontaneously.
Neuroma (scarred nerve): nerve has torn and healed with scar, compressing fibres and limiting signal transmission.
Rupture: nerve is torn distally but still attached to the spinal cord, often requiring grafting.
Avulsion: root pulled away from spinal cord (preganglionic) with no possibility of direct repair; treated with nerve transfers and muscle transfers.
Diagnosis
Accurate diagnosis requires correlation of clinical, electrodiagnostic, and imaging findings.
Detailed neurological exam maps motor and sensory deficits to specific roots/trunks and assesses associated vascular or skeletal injuries.
Electrodiagnostic tests:
Nerve conduction studies and EMG assess the extent of denervation and reinnervation and help distinguish neuropraxia from more severe lesions.
MRI (including MR neurography):
High‑resolution MRI demonstrates root avulsions (pseudomeningoceles), nerve ruptures, neuromas, and inflammation; it has good sensitivity (~88–93%) and accuracy for detecting brachial plexus pathology.
CT myelography remains the reference for detecting root avulsions in some centres.
Timing is critical; exploration and reconstruction are often indicated within 3–6 months of injury for best outcomes.
Treatment Options
Management is tailored to severity and time since injury.
Non-surgical management:
Mild stretch injuries (neuropraxia) often recover spontaneously over weeks to months with physiotherapy, pain control, and close monitoring.
Pain management, splinting, and rehabilitation for partial injuries.
Surgical reconstruction (usually 3–6 months after injury in adults, earlier in infants when indicated):
Neurolysis: freeing a nerve from scar tissue when continuity is preserved.
Direct repair: primary end‑to‑end suture in sharp lacerations with minimal gap.
Nerve grafting: bridging gaps with autologous nerve grafts (e.g., sural nerve, vascularized ulnar nerve graft) in ruptures to restore continuity.
Nerve transfers (neurotization): coapting an expendable donor nerve or fascicle to a denervated but more important nerve to reinnervate key muscles (e.g., spinal accessory to suprascapular, intercostals to musculocutaneous, ulnar/median fascicles to biceps/brachialis).
Functioning free muscle transfer (FFMT): transplantation of a free muscle (e.g., gracilis) with its nerve and vessels to restore elbow flexion or finger function when native musculature is irrecoverable.
Secondary soft‑tissue and skeletal procedures (tendon transfers, osteotomies, joint fusions) to refine function and positioning at later stages.
Reconstructive strategy depends on level (preganglionic vs postganglionic), number of roots avulsed, and patient goals.
The Procedure
At The Brain and Spine Centre:
Initial assessment: trauma work‑up, detailed brachial plexus exam, MRI and electrodiagnostics, and classification of injury pattern (e.g., C5–6, C5–7, pan‑plexus).
Operative planning: supraclavicular and infraclavicular exploration under microscope to identify viable roots, trunks, and cords; intraoperative nerve stimulation to assess function.
Reconstruction: combination of nerve grafts and nerve transfers to prioritise shoulder abduction/external rotation, elbow flexion, and hand function depending on lesion level and donor availability.
Recovery & Aftercare
Results You Can Expect
Outcomes vary widely depending on lesion pattern, timing, and reconstruction strategy.
For upper plexus (C5–6 ± C7) injuries, nerve grafts and transfers can restore useful shoulder abduction and elbow flexion in a high percentage of patients.
Results are more guarded in pan‑plexus injuries (C5–T1 avulsions), but modern nerve transfer combinations and free muscle transfers can still provide protective sensation, some elbow flexion, and improved positioning of the arm.
Early reconstruction (within 6 months) generally yields better functional outcomes than delayed surgery.
Why Choose The Brain and Spine Centre
Led by Dr. Muhammad Aqeel Natt, with specific expertise in brachial plexus exploration, nerve grafting, nerve transfer, and complex peripheral nerve reconstruction. Access to high‑resolution MRI, EMG, and CT myelography for detailed injury mapping. Individualised surgical planning focused on restoring priority functions (shoulder, elbow, hand) and integrating with a comprehensive rehabilitation program. Collaboration with orthopaedics, physiotherapy, pain management, and rehabilitation for long‑term functional maximisation.
Cost of Brachial Plexus Injury Treatment
Frequently Asked Questions (FAQs)
Can I know Dr. Muhammad Aqeel Natt’s credentials?
What types of brain tumours do you treat?
Is the surgery safe?
Do I need long-term follow-up after surgery?
Are you having health problems? Contact us today!
Address Business
Contact With Us
Call Us 24/7: 0318 4065914
Working Time
Sunday: 8.30am - 19.30pm

