At The Brain and Spine Centre, we specialize in the diagnosis and surgical treatment of neurological and spinal disorders. Dr. Muhammad Aqeel Natt, a leading neurosurgeon in Lahore, provides advanced, safe, and compassionate care for patients.

Skull Base Tumors (Surgery)
Skull base tumors require prompt, expert diagnosis and specialized surgical treatment to preserve neurological function and improve outcomes. At The Brain and Spine Centre, Dr. Muhammad Aqeel Natt provides advanced care for skull base tumors at Farooq Hospital, West Wood Branch, Lahore, combining cutting-edge neurosurgical expertise with compassionate support.
Our goal is simple: remove tumor safely, protect critical brain structures, and guide recovery for the best possible quality of life.
What Are Skull Base Tumors?
Skull base tumors are abnormal growths located between the brain and the underlying skull at the base of the cranium. Most skull base tumors are not brain tumors themselves but arise from the coverings of the brain (meningiomas), nerve coverings (schwannomas), or bones and cartilage of the skull base. These tumors can be benign (non-cancerous) or malignant (cancerous) and are categorized by tumor type and location within the skull base.
Common types of skull base tumors include:
Meningiomas growing from the brain’s protective lining, acoustic neuromas (vestibular schwannomas) arising from hearing and balance nerves, chordomas developing in skull base or spine bones, chondrosarcomas occurring in bones or cartilage, pituitary adenomas of the pituitary gland, craniopharyngiomas near the pituitary gland, glomus tumors around the jugular vein, and paragangliomas.
Symptoms of Skull Base Tumors
Symptoms depend on tumor size, location, and which nerves or brain structures are affected.
Common skull base tumor symptoms include:
Headaches and neck pain, vision changes including blurred vision, double vision, or vision loss, hearing problems such as hearing loss, ringing in ears (tinnitus), or “whooshing” sound, balance difficulties or problems walking, facial numbness, tingling, or facial paralysis, difficulty swallowing or voice changes including hoarseness, nosebleeds or nasal congestion, loss or change in sense of smell, cognitive or personality changes, and seizures.
Diagnosis
Diagnosis begins with comprehensive neurological examination testing vision, hearing, balance, facial sensation, and cognitive function.
Imaging studies are essential:
Magnetic Resonance Imaging (MRI) is the preferred imaging test for skull base tumors, providing highly detailed images of soft tissues, tumor characteristics, and relationship to surrounding structures. High-resolution MRI should be performed at 1.5 Tesla minimum, ideally at 3.0 Tesla for better signal-to-noise ratio and resolution of small structures.
Computerized Tomography (CT) scan is the modality of choice for delineating fine bony detail, detecting calcifications, and identifying bone destruction or erosion. CT and MRI are complementary and often used together to diagnose, plan surgery, and study the tumor.
Additional testing may include PET scans to locate cancer cells, hearing tests, vision examinations, and biopsy for tissue diagnosis.
Treatment Options
Observation: Small, benign tumors causing no symptoms may be managed with watchful waiting and regular imaging surveillance.
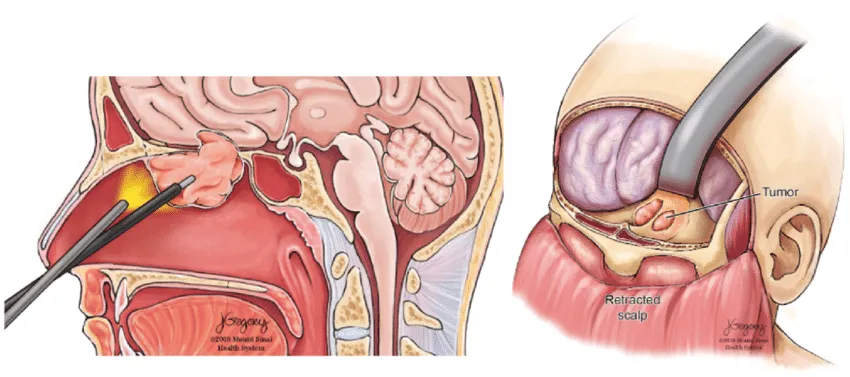
Surgery: Surgical removal is the primary treatment for most skull base tumors when symptoms are present or tumors are growing. Modern skull base surgery employs advanced techniques to access these challenging locations while minimizing brain manipulation and preserving neurological function.
Surgical approaches include:
Endoscopic transnasal surgery is a minimally invasive approach through nasal passages offering exposure of the entire anterior and central skull base without external incisions.
Pterional approach provides access to the frontal and temporal lobes and is one of the most versatile skull base approaches.
Orbitozygomatic approach extends the pterional approach by removing additional bone from the orbital rim and zygomatic arch, providing wider exposure while reducing brain retraction.
Transsphenoidal approach accesses pituitary region tumors through the nasal passages and sphenoid sinus.
Lateral suboccipital approach provides access to posterior skull base tumors.
Radiation therapy: Radiation may be used as sole therapy for certain tumor types, after surgical resection for residual tumor, or for recurrent tumors. Options include fractionated radiotherapy delivered daily over weeks, or stereotactic radiosurgery delivering a single high-dose of focused radiation.
The Procedure
Our process safeguards safety, functional preservation, and optimal outcomes:
Consultation: Comprehensive evaluation including neurological examination, symptom assessment, and imaging review to determine tumor type, location, and optimal surgical approach.
Imaging: Advanced MRI and CT scans with thin-section multiplanar imaging to characterize the tumor, assess bone involvement, and plan the surgical trajectory.
Surgery: Carefully planned approach using advanced microsurgical techniques, intraoperative monitoring, and neuronavigation to achieve maximal tumor resection while protecting vision, hearing, facial nerve function, and other critical structures.
Recovery: Inpatient monitoring typically 3-10 days in the hospital, followed by continued recovery at home.
Recovery & Aftercare
Recovery varies based on tumor type, location, surgical approach, and extent of resection. Most patients spend 3-10 days in the hospital after skull base surgery. At-home recovery typically requires 6-12 weeks. Significant improvement is usually seen within 3-6 months, with continued healing over months to years.
Physical, occupational, and speech therapy may be needed to restore strength, coordination, swallowing, and communication abilities. Regular follow-up appointments with neurological assessments monitor cognitive and motor function recovery. Imaging studies including MRI or CT scans are performed periodically to monitor for tumor recurrence. For pituitary tumors, endocrinology evaluations assess hormone levels and manage replacement therapy.
Quality of life typically improves gradually during the first year after surgery with stability during the second year. Studies show 38% of patients report significant improvement in overall quality of life, 36% report no change, and 26% report worsening. The overall quality of life in the majority of patients can be classified as “good,” with significant improvement within 12 months following surgery.
Results You Can Expect
Successful tumor removal with benign tumor surgery success rates as high as 90-95%, especially when tumors are fully removed. Skull base meningiomas can be operated upon with good outcomes comparable to other brain tumor locations. Mortality rates for skull base tumor surgery range from 1.0% to 4.7%, with complication rates of 28-47%.
Preservation of neurological function through advanced surgical techniques minimizing damage to critical structures. Studies show 76% of patients report good to moderate recovery at one year postoperatively.
Relief of symptoms as tumor compression on nerves and brain structures is alleviated.
Low recurrence rates with complete surgical resection, particularly for benign tumors. After complete resection of benign meningiomas, recurrence-free rates reach 98% at 5 and 10 years.
Gradual quality of life improvement with most patients returning to previous occupations within two years, though 75% return to preoperative baseline quality of life levels.
Why Choose The Brain and Spine Centre
Led by Dr. Muhammad Aqeel Natt, specialist neurosurgeon with extensive expertise in complex skull base surgery and microsurgical techniques. Access to advanced imaging technologies including high-field MRI and CT for precise diagnosis and surgical planning. State-of-the-art operating capabilities with intraoperative monitoring and neuronavigation for maximal tumor resection and functional preservation. Multidisciplinary team approach coordinating neurosurgery, otolaryngology, neuro-oncology, radiation oncology, and rehabilitation services. Convenient location at Farooq Hospital, West Wood Branch, Lahore with comprehensive skull base surgery capabilities.
Cost of Glioma Treatment
Costs vary with tumor type, size, surgical approach complexity, need for radiation therapy, duration of hospitalization, and rehabilitation services. Personalized estimates provided after consultation and imaging evaluation.
Frequently Asked Questions (FAQs)
Can I know Dr. Muhammad Aqeel Natt’s credentials?
What types of brain tumours do you treat?
Is the surgery safe?
Do I need long-term follow-up after surgery?
Are you having health problems? Contact us today!
Address Business
Contact With Us
Call Us 24/7: 0318 4065914
Working Time
Sunday: 8.30am - 19.30pm

